A: The FDA regulates face masks, including cloth face coverings, and surgical masks as medical devices when they are marketed for medical purposes. Medical purposes include uses related to COVID-19, such as face masks to help stop the spread of disease, surgical masks, and surgical masks with antimicrobial/antiviral agents. Face masks marketed to the general public for general non-medical purposes, such as for use in construction and other industrial applications, are not medical devices.
A: Masks may help prevent people who have COVID-19 from spreading the virus to others. The CDC recommends people wear face masks in public settings, especially when other social distancing measures are difficult to maintain. Wearing a face mask may limit exposure to respiratory droplets and large particles and may help prevent people who have COVID-19 from spreading the virus.
A: If worn properly, face masks, surgical masks, or respirators may reduce the chance of spreading a COVID-19 infection between you and those around you. The CDC provides information on Using PPE and Considerations for Wearing Masks.
FDA-cleared surgical masks and respirators have been used by health care personnel for years and have been worn in health care facilities during extended procedures without harm to the wearer. Health care personnel with medical conditions should discuss concerns they may have with wearing respirators with their own health care providers. Health care personnel should follow the manufacturer's instructions and their facility's policies for use of all PPE.
A: Source control refers to use of cloth face coverings or face masks to cover a person's mouth and nose when they are talking, sneezing, or coughing to reduce the likelihood of transmission of infection by preventing the spread of respiratory secretions. COVID-19 may be spread by individuals who may or may not have symptoms of COVID-19.
The general public's use of cloth face coverings made from common, easily accessible materials are an additional voluntary public health approach to help slow the spread of COVID-19. The CDC has information on the Use of Masks to Help Slow the Spread of COVID-19 for the general public.
Face masks intended for a medical purpose, such as prevention of infectious disease transmission, are subject to FDA regulation. The FDA has issued an emergency use authorization (EUA) as well as guidance on regulatory flexibility for such products. For more information, see "I'm interested in manufacturing face masks or surgical masks for the COVID-19 pandemic. What do I need to do?"
For more information on source control, see the CDC's Interim Infection Prevention and Control Recommendations for Healthcare Personnel During the Coronavirus Disease 2019 (COVID-19) Pandemic.
A: During the COVID-19 public health emergency, the CDC recommends health care personnel wear face masks at all times while they are in the health care facility, including in breakrooms or common areas where they might encounter co-workers or visitors.
When available, surgical masks (a specific type of face mask) are preferred over cloth face coverings for health care personnel as surgical masks offer both source control and protection for the wearer against exposure to splashes and sprays of infectious material from others.
- Cloth face coverings should NOT be worn instead of a respirator or surgical mask if more than source control is needed.
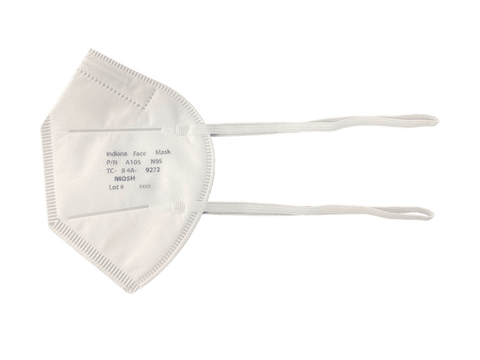
- Wear an N95 or equivalent or higher-level respirator, instead of a face mask, for:
- Aerosol generating procedures (refer to "Which procedures are considered aerosol generating procedures in healthcare settings?" on the CDC's Clinical Questions about COVID-19: Questions and Answers page).
- Surgical procedures that might pose a higher risk for transmission if the patient has COVID-19 (for example, that generate potentially infectious aerosols or involve anatomic regions where viral loads might be higher, such as the nose and throat, oropharynx, or respiratory tract). Refer to "During the COVID-19 pandemic, are there special considerations for surgical and other procedural care settings, including performance of aerosol-generating procedures (AGPs)?" on the CDC's Clinical Questions about COVID-19: Questions and Answers page.
- Health care personnel should consult their institutional policies for further guidance on what type of face mask or respirator to use.
The CDC provides information on infection control measures for COVID-19 on its Clinical Questions about COVID-19: Questions and Answers page.
A: Face masks and surgical masks are designed to serve as protective barriers and may still offer some protection even if they are used beyond the manufacturer's designated shelf life or expiration date. If there is no date available on the face mask label or packaging, facilities should contact the manufacturer. The user should inspect all masks prior to use and, if there are concerns such as degraded materials (such as elastic) or visible tears, the product should be discarded. For additional information please refer to the CDC's Strategies for Optimizing the Supply of Facemasks.
A: The CDC does not recommend the reuse of disposable surgical masks that are intended to be used once. The FDA recognizes that there may be availability concerns with surgical masks during the COVID-19 public health emergency, but there are strategies to conserve surgical masks.
A: The CDC considers N95-type FFRs a one-time-use product and recommends that cleaning, decontamination, and subsequent reuse of FFRs should only be used when there is a critical shortage of FFRs and should only be performed on NIOSH-approved FFRs without exhalation valves. For additional details, see the CDC's Recommended Guidance for Extended Use and Limited Reuse of N95 Filtering Facepiece Respirators in Healthcare Settings and the CDC's recommendations on Implementing Filtering Facepiece Respirator (FFR) Reuse, Including Reuse after Decontamination, When There Are Known Shortages of N95 Respirators.
The FDA has issued Emergency Use Authorizations (EUAs) for devices that decontaminate certain respirators. Health care facilities should check the Decontamination Systems for Personal Protective Equipment EUAs for the most up-to-date information.
FFR decontamination may be an effective method of reducing the pathogen burden. The process used by EUA-authorized decontamination devices should not harm the fit or filtration performance of the FFR and should present no residual chemical hazard to the FFR user. For additional details, see the FDA's Recommendations for Sponsors Requesting EUAs for Decontamination and Bioburden Reduction Systems for Surgical Masks and Respirators During the Coronavirus Disease 2019 (COVID-19) Public Health Emergency.
A: EUAs authorize the use of medical devices that are not FDA-cleared or approved. The EUA authority allows the FDA to help strengthen the nation's public health protections against emerging infectious disease threats by facilitating the availability and use of medical devices needed during public health emergencies.
Under the Federal Food, Drug, and Cosmetic Act (FD&C Act), the FDA Commissioner may authorize the emergency use of an unapproved or uncleared medical product or an unapproved / uncleared use of an approved/cleared medical product for certain emergency circumstances after the HHS Secretary has made a declaration of emergency or threat justifying emergency use. The FDA Commissioner may issue an EUA to authorize a medical product for use in an emergency to diagnose, treat, or prevent serious or life-threatening diseases or conditions when there are no adequate, approved, or available alternatives. The Emergency Use Authorizations (EUAs) for diagnostic, non-diagnostic, and therapeutic medical devices that the FDA has issued related to COVID-19 may be revised, terminated, or revoked as needed.
For details on the Emergency Use Authorizations for these devices, see:
- Personal Protective Equipment EUAs
- Face Mask EUA (PDF - 98KB)
If you need help with the EUA process for face masks, surgical masks, or respirators, contact CDRH-NonDiagnosticEUA-Templates@fda.hhs.gov.
There are currently no FDA-approved face masks, surgical masks, or respirators. To identify FDA-cleared face masks, surgical masks, and respirators, search the 510(k) Premarket Notification database.
A: The FDA issued an umbrella EUA in response to insufficient availability of disposable, single-use surgical masks. This EUA established performance criteria for the surgical mask to be authorized for use in health care settings by health care personnel as PPE.
Performance criteria that must be met include liquid barrier performance, particulate filtration efficiency, air flow resistance, and use of biocompatible, non-cytotoxic, non-irritating, and non-sensitizing materials. Surgical masks that have been confirmed by the FDA to meet the criteria are listed in Appendix A of the EUA as authorized surgical masks.
To be added to Appendix AExternal Link Disclaimer, test reports must be submitted to the FDA demonstrating that the surgical mask meets the performance criteria. Requests can be submitted to the FDA with the subject line "Surgical Masks EUA" to CDRH-nondiagnosticEUA-templates@fda.hhs.gov. The Surgical Masks EUA Template for Addition to Appendix A (DOCX - 56KB) can be used to provide the required information.
Manufacturers, importers, and distributors must also comply with the conditions of authorization found in Section IV of the EUA Letter of Authorization (PDF - 101KB).
The following surgical masks are not covered in the scope of this EUA:
- Surgical masks that are FDA-cleared
- Surgical masks that are manufactured in China
- Surgical masks that include drugs, biologics, nanoparticles, or antimicrobial/antiviral agents
A: The FDA does not have a list of all counterfeit or fraudulent products. To report fraudulent COVID-19 products to the FDA, email FDA-COVID-19-Fraudulent-Products@fda.hhs.gov. The CDC provides information on identifying counterfeit respirators at Counterfeit Respirators / Misrepresentation of NIOSH-Approval.
A: The FDA encourages reporting of any adverse events or suspected adverse events experienced with face masks, surgical masks, or respirators.
- In general, device manufacturers, importers, and device user facilities (health care facilities) must comply with the applicable medical device Mandatory Reporting Requirements: Manufacturers, Importers and Device User Facilities.
- Voluntary reports from health care personnel and users can be submitted through MedWatch, the FDA Safety Information and Adverse Event Reporting program.
- Health care personnel employed by organizations that are subject to the FDA's user facility reporting requirements should follow the reporting procedures established by their organizations.
Information sourced from The US Food and Drug Administration